I swore off writing about psychiatry, but today’s Times features–in addition to what we all have to hope will be the Most Inane David Brooks Column Ever–Weill-Cornell psychiatrist Richard Friedman once again letting the cat out of the bag, so I can’t resist.
Writing about the latest neurodoggle, in which Helen Mayberg claims to have found a biomarker that can predict whether a depressed person will respond to drugs or CBT (really, this stuff sounds more like phrenology or palmistry every day), Friedman says this:
In fact, I used to delight in tormenting the drug company representatives when they asked me how I picked an antidepressant. I would take a quarter out of my pocket, flip the coin and say I’d let chance decide because their drug was no better or worse than their competitors’.
Now I gotta tell you–this one puts a hair across my ass. If I had a dime for every psychiatrist from Stamford to Seattle to Sydney who has accused me of inducing patients to stop taking their drugs and throw themselves under the nearest bus simply by telling them that prescribing antidepressants is a guessing game, I’d be able to make a lot of phone calls, if there were still payphones and they still cost a dime. And yet here it is, confirmed by a prominent psychiatrist on the pages of the newspaper of record in a way that I would never dream of saying: “Yeah, we just flip a coin.”
Not that I mind being yelled at, at least not too much. I mean, if you poke a polecat, you’re gonna get sprayed. But really, who’s the one who seems uncaring about the patients? The guy who raises doubts about the science behind the treatment and suggests that people do their homework before they embark on a course of drugs that work by changing their brains (maybe forever), or the guy who compares it to figuring out who kicks off in the Super Bowl?
You also have to wonder how Jeffrey Lieberman, head of psychiatry at Weill-Cornell’s uptown rival Columbia, is going to take this news. In his forthcoming book, Lieberman, in the course of assuring us that psychiatry has “matured from a psychoanalytic cult of shrinks to a scientific medicine of the brain,” claims that psychiatrists are now “empathic prescribers of medication targeted to specific diseases,” and that the drugs fit the illnesses “in a lock-and-key relationship.” Seems to me you shouldn’t have to flip a coin if that’s so.
Oh, and one more thing. Friedman uses his column to take a swipe at the National INstitute of Mental Health, which has recently (and famously) decided to double down on the bet that we can decode the brain and figure out its role in mental illness. I personally think this is a doomed undertaking–or, more precisely, that it can only succeed at the cost of redefining the human, which is more than even the most ambitious and self-assured psychiatrist would consciously take on–but it at least has intellectual integrity. If mental illnesses are medical illnesses, they are saying, then by gum we should look for them directly in biology, which is better than just punting the issue as psychiatry has done for 150 years. Sadly for many psychiatrists, however, the NIMH initiative (known as RDoC) points to something sort of embarrassing, which is that we still don’t know what mental illness is, or which ones exist. RDoC is focused on symptoms rather than diseases, and the preliminary findings are challenging the boundaries of long accepted diagnostic categories like schizophrenia and bipolar disorder, mental illnesses that are many psychiatrists’ bread and butter.
So many psychiatrists are sore at NIMH, especially because it decided to go fully public with RDoC right on the eve of the release of the DSM-5, and to use that unveiling to announce that it is moving away from the DSM style of diagnosis. Lieberman spanks NIMH director Tom Insel for his timing (and for his ideas) in his book, and Friedman joins the chorus in his column. Following up on the conclusion that some patients are more suited to talk therapy than drugs and vice versa, he wonders if we can specify which therapy is right for which patient. But, Friedman laments,
right now we don’t have a clue, in part because of the current research funding priorities from the National Institutes of Mental Health, which strongly favor brain science over psychosocial treatments. But these are important questions, and we owe it to our patients to try to answer them.
Friedman overlooks not only that RDoC, at least on paper, is committed to psychosocial research, but also that researchers have tried for nearly eighty years to answer that question, and keep coming up with the same one: that all therapies are equally effective (or ineffective). This finding even has a name: the Dodo Bird Verdict (check your Alice in Wonderland for the reference.) The only consistent effect that can be found is that success in therapy is not a function of technique but of relationship, but mostly it seem it is nearly impossible to answer the outcome question without assuming your conclusions as your premises. In other words, the research almost always shows that the researchers’ methods are the best. this may indicate that therapy is not penetrable by the scientific gaze, but Friedman decides to overlook the knotty epistemological issues here and take the easy way out. He just blames the government. And blaming NIMH for the Dodo Bird Verdict is like blaming hte National Weather Service for the weather.
And not only that, but guess who paid for Mayberg’s research? That’s right: the National Institutes of Health.










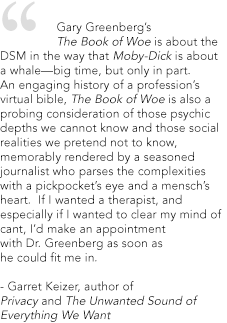
Don’t quit on psychiatry! Get into this managed care beast. I’m 77 and working on a book based on my 42 years of independent practice. What a priviledge. Indeed, the patient is the expert on his life. Loved your Book of Woe concluding comments on an honest psychiatry. That’s what I tried to do. Patients can show the way.
Good work, Gary!
The patient becomes the arbiter of patient care quality when the patient is empowered and directs $ to the doctor. That’s the health care marketplace at work. And that is a missing key to real health care funding reform.
Critics of PP argue that independent docs’ incentives push $ for them at the expense of care quality. That was patently untrue in my psychiatric practice. Here’s why:
For my psychiatric practice, I’d need to either manufacture time or arbitrarily bump up my fee if paid only by the patient for our face-to-face sessions (I chose to be on B. F.Skinner’s fixed ratio schedule; I’m not the Wizard of Oz, on LSD, or floundering in Alice’s rabbit hole and I’m unable to manufacture time in this universe). Thus, I and the patients were both “incentivized” to use B=f(x) under c (per the scientific bio-behavioral method, where x is consequences of the patient’s behavior — see Inescapable consequences by Gene Richard Moss). I charged the same fees for all patients – which were clearly posted on my practice website.
The “skin in the game” for both the patient and me was using our clinical time well (that’s my definition of doing quality psychiatric care) and evaluating (measuring) the success of that clinical time to functionally (not via DSM or ICD codes) diagnose, plan and help the patient deal with his problems as our mutual goal and modus operandi.
As we all know, schemes to pay psychiatrists and primary care physicians for their performance independent of actual patient interactions pervert the Hippocratic contract and doctor-patient relationship. ACOs and HMOs reward docs for doing less (or avoiding patients), and employed/salaried docs (especially when associated with rich pensions) must either play the hiring institution’s tune or say goodbye.
Lee H. Beecher, MD
President, Minnesota Physician-Patient Alliance (MPPA)
7574 Mariner Point
Maple Grove, MN 55311-2617
http://www.physician-patient.org
“Empowering patients and physicians to make informed health care decisions”
Phone: 763-420-4250
FAX: 763-416-4962